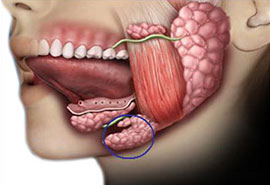
The main salivary glands are parotid, submandibular, and sublingual glands, which are also called major salivary glands. In addition, there are hundreds of minor salivary glands widely located in the mucosa, extending from the mouth to the larynx. The salivary glands produce approximately 1000-1500 cc of saliva per day.
The main diseases of the salivary glands are infections, stones, stenosis, and tumours.
Salivary Gland StonesSalivary gland stones are most commonly seen in the submandibular gland. The viscosity of the saliva produced by the submandibular gland is lower than the others, and the excretion of the gland is in the opposite direction of gravity. It is considered that all these factors cause submandibular gland stones to be more frequent. Apart from this, any decrease in salivary flow and increases in saliva pH value (decrease in acidity) may lead to stone formation. Uric acid stones can also occur in gout disease.
Complaints about salivary gland stones vary according to the location of the stone, the degree of obstruction, salivary secretion rate, and whether there is an infection in the gland. The typical complaint is sudden swelling and pain in the related gland location, especially when a food that increases salivation, such as lemon, is consumed. If there is no complete blockage in the canal, the swelling will disappear in a couple of hours. Then, when a food that stimulates the salivary gland is consumed again, the complaint reappears. The diagnosis is made by the patient's history, examination findings and radiological examinations. If the stone is close to the point where the salivary gland duct opens into the mouth, it can be felt with the fingertip during oral examination. If there is a bacterial infection associated with it, there may be an purulent discharge into the mouth with pressure on the gland. Ultrasound and computed tomography (CT) are the most commonly used radiological examinations for stones. An examination called sialography, which is performed by administering a substance from the salivary gland duct, can also be used more rarely. Another examination that can be done is MR sialography. If there is an acute bacterial infection together with the stone, first the infection is treated with antibiotics, anti-inflammatory drugs and increased fluid intake. The classical treatment of salivary gland stones is open surgical methods. If the stones in the submandibular salivary gland duct are close to the duct opening in the mouth, they can be removed intraorally. However, currently sialendoscopy has opened a new era in the treatment of salivary gland stones.
SialendoscopySialendoscopy is a method used in the diagnosis and treatment of diseases of the salivary gland ducts, and has become increasingly popular in the world in the last 20 years. In Turkey, although the number of centers where this method is applied has been increasing, sialendoscopy is still performed by a very small number of physicians.
The main application area of sialendoscopy is recurrent swelling of the salivary glands. In this method, using very thin, semi-rigid endoscopes and a camera, the salivary gland ducts are entered through their openings in the mouth, and the ducts are evaluated. Although diagnostic endoscopy can be performed with local anaesthesia, general anaesthesia is generally preferred in therapeutic sialendoscopy. The most common pathologies are stones and canal stenosis. Suitable stones can be removed with the help of baskets and some other tools. Stones with a length of 4-8 mm can first be crushed with the help of laser, or pneumatic lithotripsy, and subsequently, the fragmented pieces may be removed using baskets. In larger stones, sialendoscopy can be combined with open surgical methods. Again, using this method, it is possible to diagnose and treat stenosis that is mostly encountered in the parotid gland.
Before sialendoscopy was applied, the salivary gland, especially the submandibular gland, was traditionally sacrificed. Currently, with the use of sialendoscopy, it is expected that the number of sacrificed glands will gradually decrease. Stones in the parotid gland create a more complicated situation. Adhesions related to inflammation and infection, might render parotid surgery more risky, especially in terms of facial paralysis. If the stones in the parotid can be removed by sialendoscopy, the risks to which the patient is exposed will be minimized.
Sialendoscopy cannot be performed immediately in a patient with acute salivary gland infection. First of all, medical treatment is administered for about 10 days and sialendoscopy can be performed at least 3 weeks after the onset of the infection.
After the procedure, a thin stent can be placed in the opening of the salivary gland duct, this stent is left in place for 2-3 weeks, but sometimes the stent in question may fall spontaneously beforehand. Antibiotics and anti-inflammatory drugs are used after sialendoscopy. It is important that the patient consumes plenty of water and stays away from agents that stimulate salivary gland secretion, such as lemon, for 3 weeks.
In conclusion, sialendoscopy is an important alternative to classical surgical methods in the diagnosis and treatment of salivary gland stones and duct stenosis in appropriate cases. It is possible to use this method together with other methods when necessary.
Salivary Gland Tumours80% of salivary gland tumours originate from the parotid gland, approximately 10% from the submandibular gland, and the remainder from the sublingual and minor salivary glands. Although a large variety of tumours are encountered, 80% of the tumours in question are benign, and only 20% are malignant. The most common benign tumour is 'pleomorphic adenoma', 'Warthin's tumour' comes second. The most common malignant tumours are mucoepidermoid cancer and adenoid cystic cancer.
Typically, a pleomorphic adenoma grows slowly in the salivary gland in front of the ear, where it is most commonly located. It is a well-circumscribed mass, does not cause facial nerve palsy, and is not painful. Sometimes patients apply as soon as they notice the mass in question, and sometimes they come to the physician when they let it grow well for a few years and cause a cosmetic problem. Malignant tumours, on the other hand, grow faster, they may appear as hard masses that have little or no mobility. Sometimes they can cause facial nerve palsy. The most commonly used radiological examinations are ultrasound, MRI (Magnetic Resonance Imaging) and Computed Tomography (CT).
Then, a procedure called fine needle aspiration biopsy is performed. No anaesthesia is required in this procedure. Our pathologist colleagues can examine these cells and give us information about the type of tumour. However, biopsy performed in this way gives a 'preliminary idea', and sometimes a different result can be obtained after surgery.
The main treatment is surgery. In benign tumours, such as the majority of parotid gland tumours, the tumour is removed together with a part of adjacent gland. If the tumour we deal with is in the submandibular gland, the entire gland is removed. It is known that if a patient with a pleomorphic adenoma deny surgery, and if the tumour remains in place for more than 10 years, it can possibly turn out to become a malignant tumour. More extensive surgeries are performed in malignant tumours. The entire gland can be removed, if the patient has facial paralysis before the operation, the facial nerve is also removed with the gland, or if the tumour is found to have invaded the facial nerve during the operation, the affected part of the facial nerve can be sacrificed, and this part can be repaired with a nerve graft. Again, in some malignant tumours, the lymph nodes in the neck can be removed, and in some cases, radiation therapy may be necessary after surgery. In malignant tumours with skin involvement, the skin can also be removed and some reconstruction methods might be required.


